
A cervical screen, or smear test, takes just 5 minutes and can help us to know whether we are at risk of developing cervical cancer, yet so many of us put it off. This blog will give you more information about what’s involved, to inform your decision making.
Cervical cancer
In the UK <1% people with a cervix will develop cervical cancer. Risk factors for developing cervical cancer include:
- smoking
- combined contraceptive pill usage
- HIV
- maternal history of DES usage (a medication given to some pregnant women for miscarriage until the 70s)
Cervical cancer mortality rates have reduced by 70% since the start of the UK screening programme.
The invite for a smear test
To receive an invite automatically you need to be registered with a GP surgery, be aged between 25 and 64, and be registered as female with your GP surgery.
If you have a cervix and are not registered as female with your GP surgery the screening is definitely still recommended and although you will not be sent an automatic invite you can request an appointment from your GP surgery, and ask them to automatically invite you themselves next time. More info is available from Jo’s trust.
Invites for your screening appointment are sent by post from the screening office, so do keep your address up to date with your GP. If you don’t book after the first invite the screening office will send a reminder 18 weeks later. They then let your GP know if you haven’t taken up the offer, and your GP surgery may well then text you or contact you directly by phone or letter.
The interval between appointments depends on your previous result, and may be 1 year, 3 years or 5 years. Or you may be invited direct to colposcopy for an additional examination.
Screening rates are falling, and currently nearly 1 in 3 people eligible for cervical screening don’t take up the invite. There can be many different factors that contribute to this, including difficulties in getting appointments through to experiences of pain with the appointment, embarrassment of the test itself, and fear of what the results may show. Rates of uptake are known to be lower for those with a disability, those who do not have English as their first language and those over the age of 50.
Symptoms to report
Any new symptoms such as a change in vaginal bleeding or persistent vaginal discharge should be checked with your GP or ANP. Don’t just book for a cervical screening appointment.
The smear test itself
The testing has changed over the last few years, and now in England, Scotland and Wales the cervical screening test checks for the HPV virus. If certain types of the virus are present then checks are made on the cells themselves. This has made the test more accurate for us, and means less of us will need to have further examinations.
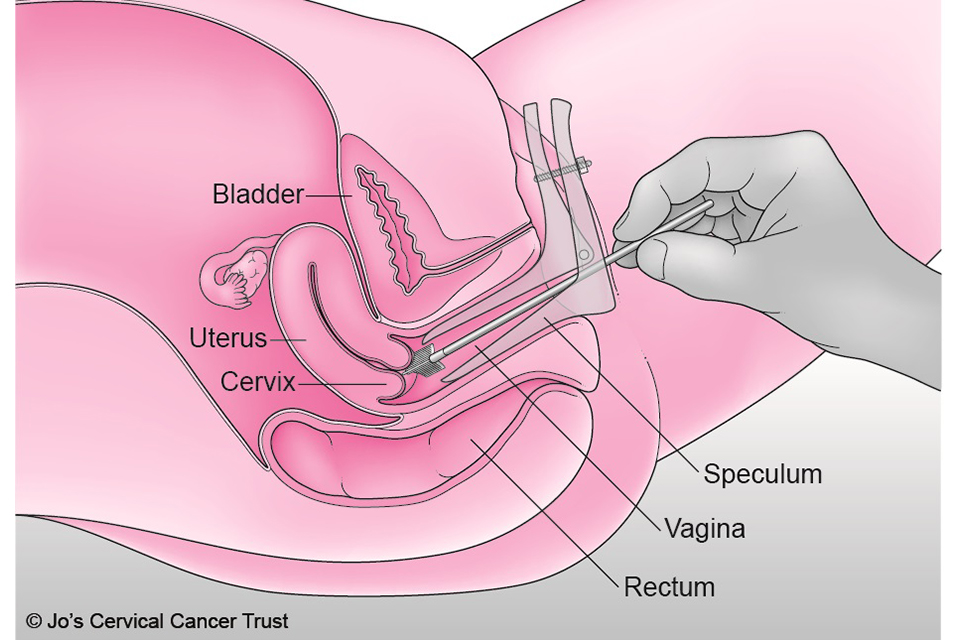
The testing is done via a speculum examination. Depending on the position of your womb (uterus), the clinician may ask you to raise your hips by placing your hands under your buttocks. Our wombs are all positioned differently, and the position can vary through the menstrual cycle, don’t be worried if you are told yours is tilted!
The sample is sent to the lab and the results are then sent to you directly by post, so do make sure your GP surgery has the correct contact details for you to receive your results. You should get your results within 2 weeks and your GP surgery will receive a copy of the results when you do.
HPV
Human papillomavirus (HPV) is a very common virus, and most of us will have it at somepoint in our lives. It is transmitted through skin to skin sexual contact. HPV can infect the skin and any moist membrane, including the cervix, vagina, vulva, anus and mouth. There are over 200 types of strains of HPV, and <10% of the strains are linked with the development of cancer.
90% of the time when we have HPV it goes away within 2 years without causing any problems.
On occasion though it can be persistent, and if this is with a higher-risk strain it can lead to pre-cancerous changes in cervical cells. HPV is more likely to be persistent if we smoke. We don’t know when we have HPV or pre-cancerous changes in cervical cells, which is why the screening test for persistent high risk strains is so useful for us.
>99.5% of cervical cancer is caused by HPV. Pre-cancerous cell changes can usually be treated effectively.
Young people are now offered HPV vaccines at school. The screening programme is still recommended even if a young person has received the vaccine. The current vaccine being used protects against 9 types of HPV, which cause >95% of cervical cancers.
Your cervical screening results
When you receive your results you may see
- HPV negative – no further tests needed, “routine” recall e.g. 3 years
- HPV positive, no abnormal cells present – no further tests needed, “sooner” recall e.g. 1 year
- HPV positive, abnormal cells present – you will be automatically referred for a colposcopy, an extra examination to further assess (and treat) the abnormal cells
- Inadequate – the sample could not be analysed well enough to give a reliable result – you will be asked to attend for a further test in 3 months time
Cervical screening at menopause
The rate of screening in those over the age of 50 is at an all-time low. A survey by Jo’s Trust of those over 50 reported that 29.1% of women over 50 had found the screening test painful since becoming older.
The genito-urinary syndrome of the menopause (GSM) can be treated though. For cervical screening the use of local, vaginal oestrogen for at least 2 weeks prior to the test can make a considerable difference. Different labs will have different guidelines about when treatment needs to be stopped before the test – usually a few days. You can check with the practice nurse at your surgery.
GSM can also mean we are more liekly to receive an “inadequate” result, which can be extremely frustrating, especially if the procedure was painful.
Top tips if you’re worried about attending for a cervical screen
If you can, do try to share any worries you have about the test with the clinician. They are very likely to have heard those same worries before, and can give you some personal advice.
These things sometimes help:
- You can ask for a chaperone.
- You can ask for a clinician of a particular gender.
- You can bring a friend to the appointment
- You can bring something to listen to during the appointment.
- Wearing a dress or skirt may help you feel less exposed. It’s fine to keep your socks on!
- Try to prioritise the appointment in your diary, as you would for a child or partner’s essential healthcare appointment.
It can be very difficult to attend for a screening appointment if you have experienced any type of sexual violence in the past. You can book an appointment to talk the test through, to see whether there is a way the appointment can go ahead in a manner that works for you. Sometimes people like to see/feel the speculum, sometimes people prefer to insert the speculum themselves with the clinician then taking the test.
The future of smear tests
Hopefully soon cervical screening tests will be done at home with a self-sampling kit. The You Screen study trialled this in certain parts of the UK in 2021.
There are private kits available to buy online, but the results of these are not acted on by the NHS screening programme, so it is best to attend your GP surgery for screening if you feel able to.
Whether or not to attend is your choice, you can opt in or out of the screening programme at any time.
Cervical screening is certainly a test I’d recommend if you feel able to attend.
For more info..
What is cervical screening – NHS
Colposcopy information – Jo’s Trust
Macmillan – Cervical screening awareness week
HPV vaccine – NHS website
Vaginal dryness – Women’s Health Concern
