A Guide to Menstrual Health
There are many questions and misconceptions about the menstrual cycle. From period pain to hormone fluctuations, it’s crucial to understand what’s normal and what might be worth discussing with a healthcare professional. In this post, we’ll explore key aspects of menstrual health, including cycle length, pain, heavy menstrual bleeding, and much more.
What is Menstrual Health?
On average you’ll have around 450 periods in your lifetime. One person’s experience of menstruation is their only experience. We don’t know what someone else’s normal is, we don’t know if our experiences are normal. To be able to identify if something’s wrong, we need to start with an understanding of what’s normal. I’m going to try and help you make sense of the menstrual cycle, for you and your friends/daughters/colleagues.
So, let’s begin with the basics: What is a “normal” menstrual cycle?
What is a Normal Menstrual Cycle?
It’s important to know that only about 10% of people have a 28-day cycle. A normal cycle can range from 24 to 38 days, with most people experiencing periods lasting between 4 and 7 days.
Irregular periods are common, especially during times of hormonal transition, such as puberty and perimenopause. Irregular periods can also occur with changes in weight, stress levels, or underlying health conditions like PCOS (Polycystic Ovarian Syndrome) and RED-S (Relative Energy Deficiency in Sport).
What are the Different Stages of the Cycle?
The menstrual cycle is divided into different phases. Here’s a quick breakdown:
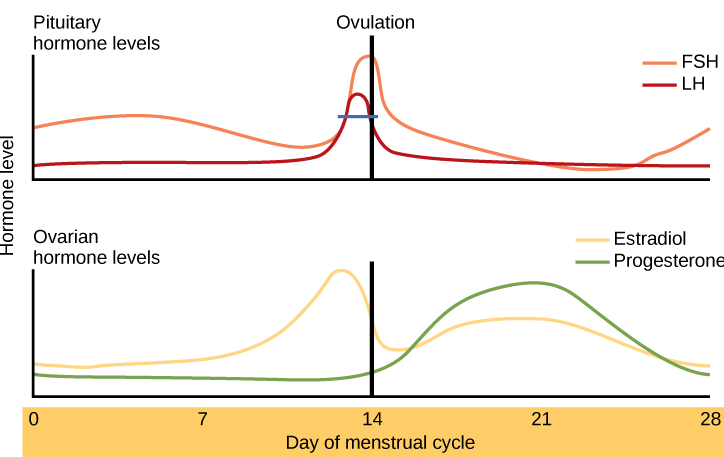
The first day of your period marks the start of the follicular phase, which is more oestrogen dominant. This phase lasts until ovulation.
Ovulation occurs on day 14 in a 28-day cycle. Testosterone surges just before ovulation, so our libido peaks just as we are most fertile, and then from ovulation oestrogen and testosterone fall.
After ovulation, is the more progesterone dominant luteal phase. Progesterone peaks 7 days before our next period and then in the few days before our next period, we may experience PMS symptoms as our hormone levels fall. In our language, we talk about PMS as when we are hormonal, but actually, it’s related to hormone levels falling.
Should You Expect Some Period Pain?
In terms of period pain, we have hormone-like substances called prostaglandins in the womb, and these trigger the period through contractions of the womb. They also regulate how much blood we lose. It’s the prostaglandin effects that can lead to cramps, aswell as other effects like looser stools.
Pain that interferes with our daily activities though is not expected, we shouldn’t be feinting with our periods, or having to take time off work or college. Pain that affects us like this may indicate a medical condition like endometriosis, where cells similar to the ones in the lining of the womb grow elsewhere in the body.
How Do You Know if Your Bleeds Are Heavy?
A typical period involves a blood loss of around 5 to 80 mls. If you’re losing more than that, it’s considered heavy menstrual bleeding. This can mean needing to change period products after 1-2 hours, needing to double up on period products, flooding through clothes or experiencing a bleed lasting longer than 8 days.

Heavy bleeding can be due to fibroids, polyps, or adenomyosis. It’s also common during perimenopause. Heavy menstrual bleeding commonly leads to anaemia and can affect your quality of life, energy levels and cognition.
Does Everyone Get PMS?
Around 90% of people who menstruate will experience some form of PMS (premenstrual syndrome). There are over 150 physical, emotional and behavioural symptoms ranging from breast tenderness to lack of co-ordination to bloating. For about 30% of people, PMS can be more severe. Additionally, PMDD (Premenstrual Dysphoric Disorder), a more severe form of PMS, affects 5-8% of people and can cause extremely distressing symptoms.
How Does Hormonal Contraception Affect the Menstrual Cycle?
Hormonal contraceptives, like pills, injections, or implants, essentially pause your menstrual cycle. The bleeding you experience on the pill isn’t technically a period; it’s a withdrawal bleed, induced by the hormone-free week of the pill. A hormonal coil (like a Mirena) may or may not stop ovulation and typically leads to lighter or absent periods. So with a pill we bleed but don’t cycle, and with a Mirena we cycle but don’t bleed.
Why Track Your Cycle?
Tracking your cycle can help you tune into your body and gain a better understanding of your unique cycle. By keeping track of symptoms over 2-3 months—using a diary or a tracking app—you can start to recognize physical and emotional shifts at different points in your cycle. The whole cycle and parts of the cycle, particularly the follicular phase, can vary in length and experience from cycle to cycle as well as over time. The luteal phase tends to be more consistent and typically lasts 14 days.
After a few months of tracking you may have a sense of your typical experiences at each stage, and may be able to use this understanding to plan work, exercise and rest around it. It may not always be predictable, especially at perimenopause, and there will be some things you can’t change, but you’ll have more awareness and hopefully feel more in control.
Should You Change Your Nutrition with Your Cycle?
Hormones can influence appetite and metabolism. In the follicular phase, as oestrogen rises, many people experience a suppressed appetite. However, in the luteal phase, progesterone levels increase and appetite tends to rise, often leading to food cravings.

Here’s how you can tailor your nutrition to support your cycle:
- During your period, focus on a whole-food, plant-based diet rich in iron and vitamin C to optimize iron absorption. Fruits, veggies, pulses, nuts and seeds are excellent options. Many people will get gut symptoms with their period, so limiting foods that stimulate the gut like coffee, alcohol, fatty and spicy meals, can be helpful.
- In the follicular phase, your metabolism speeds up, you need more calories and you are primed to access carbohydrates for fuel.
- In the luteal phase, your body burns more fat for fuel. Fats like those in avocados, nuts, seeds, and olive oil, can support hormone production.
- Omega 3 (oily fish, nuts and seeds); Magnesium (nuts and seeds, dark chocolate, pulses, banana, avocado, and leafy greens); and zinc (wholegrains, pulses, dairy, nuts and seeds) can be helpful for PMS symptoms. You may find it helpful to limit caffeine, alcohol and ultraprocessed foods to support PMS too.
What About Exercise?
In terms of movement, well hormones impact your body in so many ways – from metabolism, how well you tolerate heat, reaction time, breathing rates, muscle cell turnover, and more.
When we think of how we may want to move with our period, there are no set rules. Some people will be low on energy and may prefer yoga, and low intensity workouts. Other people may have lots of energy and can really go for it at this time. Paula Radcliffe broke the world record for the marathon while she had menstrual cramps! When you exercise your body increases endorphins, which can help with period pain.

In the follicular phase we tend to be motivated, and can adapt well to intense training. There is some evidence to say injuries are more common at this time though. More strength training in the follicular phase can lead to up to 15% more strength gains than spreading training evenly throughout the cycle.
Often in the luteal phase, we may have less motivation. This can be a great time for slow and steady endurance-type activities such as yoga, although we can sometimes feel more clumsy or uncoordinated.
In the pre-menstrual phase it can be good to build in some feel-good energy lifting and anxiety-relieving movement practices, perhaps a dance in the kitchen or a walk outside in nature.
Is Sleep Affected by the Cycle?
Yes, our sleep is affected by our hormones. Both oestrogen and progesterone can support restorative sleep. It varies with our menstrual cycle, typically being at its best just after ovulation in the middle of the cycle, and at its most disturbed at the end of the luteal phase just before and then during our period.
Resources for Further Information
If you want to dive deeper into menstrual health, here are some great resources:
- Period Power by Maisie Hill.
- BBC Radio 4 – 28 ish Days Later
- “Just a Period” – Wellbeing of Women
- The Lowdown
- PMS and PMDD support
- Endometriosis UK
- Verity PCOS UK
- Project RED-S
By understanding the menstrual cycle and tracking its patterns, we can better navigate the ups and downs of each phase, making informed choices for our health and well-being. Listen to your body and seek advice when something doesn’t feel right.
