Following on from last month’s blog about the menstrual cycle, let’s take a deeper look at hormones—how they impact our health and why understanding them is crucial, especially when we are navigating hormonal transitions like menopause.
I want to start by acknowledging that not all women were assigned female at birth and that some trans men and non-binary people will also experience these hormonal effects.
Table of Contents
The Gender Health Gap: Why We Need to Talk About Hormones
Women in the UK live longer than men, but we also spend a significantly greater proportion of our lives in ill health and disability. This disparity is partly due to the lack of focus on hormones and the underrepresentation of women in clinical trials. For years, the male body has been the “default” in healthcare, and the male experience of illness is what we typically learn about in medical school.
When I began medical school in 1994, it had only been a year since it was mandated that women must be included in clinical research. Before that, they were usually excluded as the variability of women’s results was deemed too complicated everything. So my learning, and a whole generation of clinicians like me, was based on the male experience. This has had significant impacts on women’s health outcomes. We understand now that women respond differently to drugs, and present differently with illnesses, and hormones play a really big role in everything!
The Significance of Hormonal Transitions
Hormonal transitions are some of the most significant periods in a woman’s life. Puberty, the postnatal period, and perimenopause each bring dramatic shifts, both physically and emotionally.
Some of us, for example if we have PMS or PMDD, are particularly sensitive to fluctuations in hormone levels across the menstrual cycle and may experience much worse symptoms at hormonal transition times.
We know trauma impacts our hormonal experience too, and for example, if we have experienced childhood trauma we are more likely to experience depression at menopause.
Additionally, the diagnosis of neurodiversity in women peaks during puberty and perimenopause, times of hormonal transitions. Understanding hormones and what happens at these transitions is key to understanding why women’s experiences of health can be so different from men’s.
What Are Hormones?
Hormones are chemical messengers that have many different roles and functions. For this blog, let’s focus on three key sex hormones: oestrogen, progesterone, and testosterone. These hormones affect everything from mood and energy to metabolism and reproductive health, yet many of us don’t fully understand what they do and how they work. Let’s break it down:
Oestrogen
Oestrogen, described by Maisie Hill as the “Beyoncé” of hormones, is the hormone that makes us feel unstoppable. When we’re in an oestrogen-dominant phase, we’re typically more confident, talkative, and sociable. If we think about this through the reproductive lens, basically oestrogen helps us find a partner.
And although we probably all know about its role in puberty and reproduction, there’s so much more. Oestrogen receptors are present throughout our body, which is why it affects so many aspects of our health:
- Bone and Muscle Health: Oestrogen helps build and repair tissues, including muscle and bone. It keeps our joints supple too.
- Sleep and Mental Health: Oestrogen stimulates serotonin (the feel-good neurotransmitter), improves mood, and blocks cortisol (the stress hormone). It regulates sleep and many of us will have had worse sleep with our period when oestrogen levels are lower.
- Metabolism and Cardiovascular Health: Oestrogen helps our metabolism and reduces inflammation. It has great metabolic effects on glucose, lipids, and blood vessels and we’re really protected from cardiovascular disease by oestrogen. Oestrogen regulates nitric oxide, which is a vasodilator. This effect is one of the reasons migraines are more common in women when they have less oestrogen.
- Body Temperature: Oestrogen helps regulate body temperature, which is why many women experience hot flushes and night sweats at menopause.
- Gut Health and Allergies: Oestrogen helps the gut microbiome and maintains bowel function. Often in a menstrual cycle, we notice diarrhoea with our period when oestrogen levels are lower. It regulates our appetite, and food cravings are common when oestrogen levels are lower with your period. Oestrogen has an anti-inflammatory effect. It stimulates histamine release, which can affect allergies.
- Genito-urinary Health: Oestrogen increases libido, lubricates the vulvovaginal tissues and helps the vaginal microbiome. The most common time for thrush is just before our period when oestrogen levels are lower. Oestrogen also improves bladder function and reduces urinary infections.
- Skin and Hair: Oestrogen reduces moisture loss from our skin and produces melanin. It stimulates hair and nail growth.
So all in all, it’s pretty amazing, and no wonder we notice the effects of the levels falling, whether that’s with our period each month, or at menopause.
Progesterone

Then progesterone, well it’s quite different. So when we ovulate, the remains of the follicle in the ovary form the corpus luteum, which produces progesterone. From that reproductive lens progesterone is there to nourish us and support a pregnancy. progesterone slows everything down, we want to rest and eat. In the second half of our cycle, the progesterone dominant luteal phase we may be more introspective, craving a hot bath and an early night!
Calming for most of us, it helps us sleep. I say most because around 10% of women have quite a different experience with progesterone and find it has the opposite effects.
Progesterone also supports bone health, and the uterus lining. So if at perimenopause we don’t ovulate we will have less progesterone, our cycle will extend and we may experience spotting before our period, and then our period when it comes will be heavier and longer. In terms of mood unfortunately our bodies try to compensate for less progesterone by increasing cortisol and adrenaline, so there’s a double whammy of losing the calming effects of progesterone and gaining more cortisol.
Testosterone
Testosterone is described by Maisie Hill as the Serena Williams of our hormones. Produced by the ovaries and adrenal glands, testosterone contributes to feelings of ambition, competitiveness, and physical vitality. Testosterone levels naturally decline from our 30s. The effects of a lower testosterone are much more pronounced in early menopause and after removal of the ovaries.
Thanks to Davina testosterone is known for its effect on libido, but the other effects are still being debated. Women who use testosterone as part of HRT often report improved mood, energy, strength, memory, and vaginal health. However, studies on testosterone’s broader effects in women are still very limited, and more research is needed to confirm its full benefits.
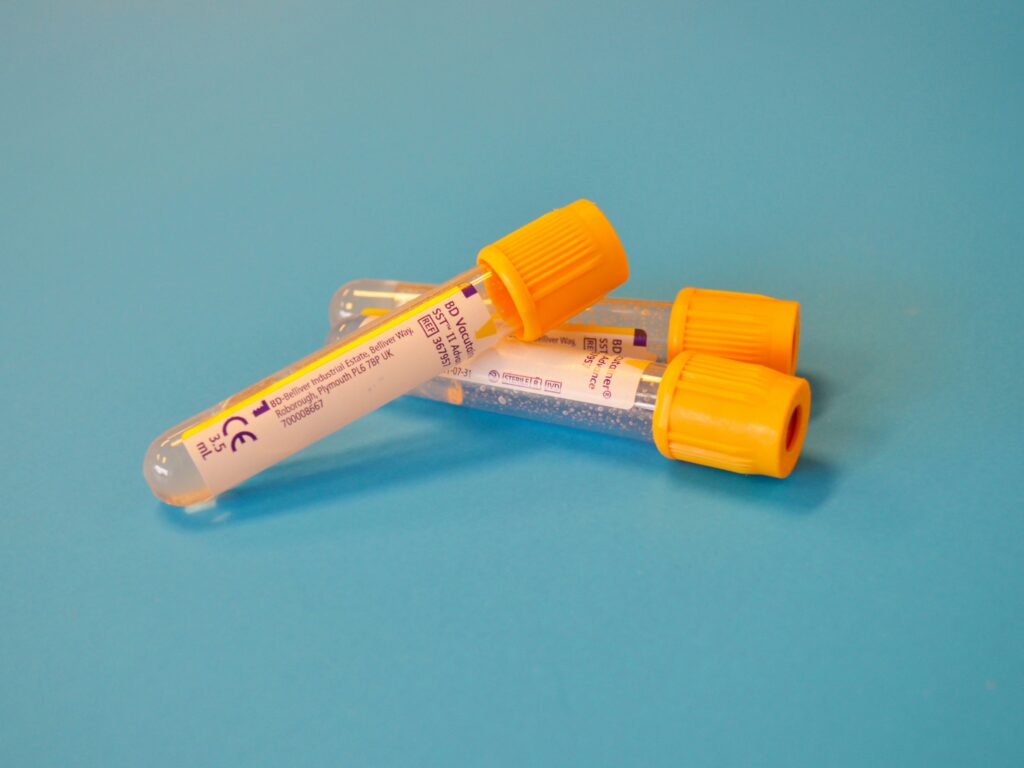
The Problem with Hormone Testing
Many women seek blood tests to understand their hormonal balance, but these tests provide limited insight. Hormone levels fluctuate throughout the day and the month, and a single test doesn’t capture your average levels over time. Tracking your menstrual cycle can offer a more accurate picture of how your hormones are performing. Your menstrual cycle is a vital sign—its length, regularity, and any changes can indicate shifts in your hormonal health.
Conclusion
Understanding your hormones is key to navigating health and wellness throughout the different stages of life. From puberty to menopause, hormonal changes influence everything from your mood to your metabolism. By learning more about how your hormones work, you can take control of your health and make informed choices that support your well-being. Here at Rethink I can support you with all queries hormone related, find out more at rethinkmenopause.com/services/.
