
Table of Contents
In my experience, bone health is not something many people are that concerned by, unless they have seen first hand how significantly osteoporosis has affected a family member. However, the implications of falls and fractures, especially for postmenopausal women, underscore the importance of proactive bone care. In the UK, 50% of postmenopausal women will break a bone, often because of osteoporosis. Even seemingly minor fractures, like a broken wrist, can disrupt daily life, affecting work, mobility, and independence.
Other fractures, particularly of the spine and hip can be potentially life-changing and even life-threatening. Women have an 11% lifetime risk of a fracture of their spine, versus 2% in men. A woman’s risk of hip fracture is the same as the risk of breast cancer, womb cancer and ovarian cancer combined. Women’s risk is higher than mens due to a number of factors – hormones, lower body weight and typically living longer being some!
The Hidden Threat: Osteoporosis and Osteopenia
Osteoporosis and osteopenia signify a reduction in bone density, often described as ‘bone thinning.’ While bones may appear normal externally and cause no immediate discomfort, this internal thinning weakens the bones, making them more susceptible to fractures. Bone health is influenced by age, gender, ethnicity, weight, alcohol, smoking, and family history. Other factors like early menopause, anything that has stopped periods (for example lower body weight or high levels of training), medical conditions (including type 1 diabetes, rheumatoid arthritis, coeliac disease), and certain medications (including high dose steroids, some cancer treatments, some epilepsy treatments and the depo-provera contraceptive injection) are also key.
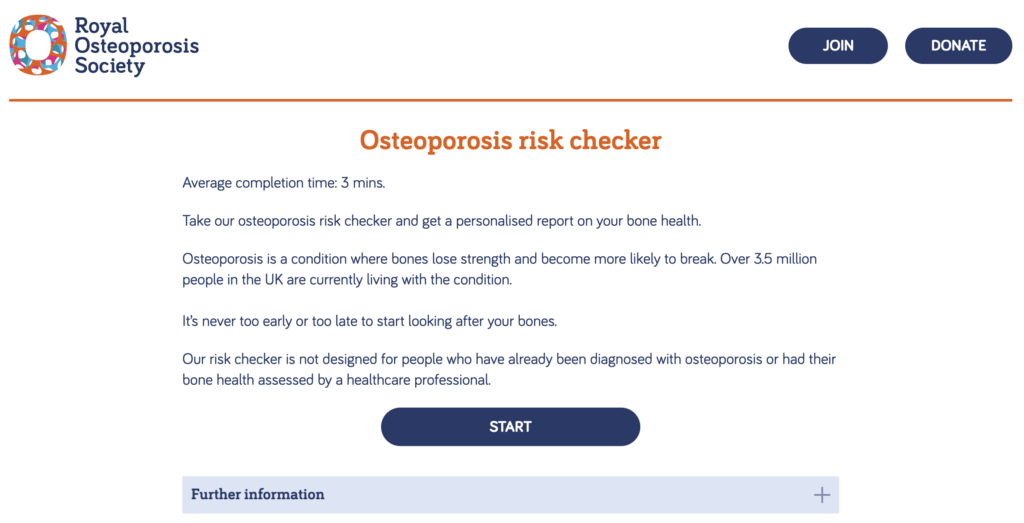
This risk checker has been produced by the Royal Osteoporosis Society and is a really useful tool that anyone can use. You can complete it online and will be emailed a report that if you wish you can share with your Menopause Specialist or GP.
In a consultation I would use a similar tool to calculate a FRAX score to assess the likelihood of fracture risk over the next 10 years and help to assess whether more information is needed, such as via organising a DEXA scan. Currently there is no national screening programme for osteoporosis, although in 2012 NICE (National Institute Clinical Excellence) did suggest that 10 year fracture risk should be estimated in all women over 65. I build this into all my consultations and health checks here at Rethink.
How does menopause affect bone health?
Bone is essentially like scaffolding, composed of essential elements such as protein, collagen, calcium, and various minerals. This living structure undergoes continuous remodelling, characterised by the breakdown of older bone tissue and the simultaneous rebuilding of new bone.
In childhood, the emphasis is on bone building, facilitating the expansion of the skeleton in size, density, and strength as we grow. Remarkably, during this phase, the entire skeleton renews itself every two years. Although bone growth halts in our late teens, maturation persists, and we reach peak bone mass during our 30s. As adults, the process of complete skeletal renewal takes approximately seven to ten years.
Up until the age of around 45, a delicate balance is maintained between the removal and creation of bone. Oestrogen has a pivotal role,its anabolic nature supporting the development of tissues, including muscles and bones. We can experience a loss of up to 20% in bone density during the five years following the last period.
It’s worth noting that men also undergo bone loss as they age, albeit in a more gradual manner compared to women.
Building Strong Bones
Promoting bone health involves a holistic approach encompassing nutrition, exercise, lifestyle choices, and, if necessary, medications. Adequate protein, along with vitamins D and K, as well as calcium, forms the foundation of a bone-friendly diet. Vitamin D supplementation of 10-20 mcg per day is recommended for everyone in the UK in the Winter months (and for some people year round) as we mainly get vitamin D from sunlight. In Spring and Summer, ensuring sun exposure for at least 20 minutes a day should meet our needs; but we may need 2 hours of exposure if we have darker skin, and may not absorb so well if we are wearing a high SPF. Leafy greens are great sources of both vitamin K and Calcium, and the Royal Osteoporosis Society has a link to a useful calcium calculator if you’re not sure you are getting enough.
Regular weight-bearing and strength training exercises contribute significantly to bone health. Weight-bearing exercises involve the skeleton supporting the body’s entire load, promoting bone density through adaptive responses to force. The impact we need to support our bone density will depend on our baseline. Someone who is sedentary will see a significant benefit from a short walk each day, but someone who is very active needs to work a bit harder. Running, jumping and tennis are great for bones. It’s worth noting that swimming doesn’t count as weight bearing exercise. We should aim for this every day.
Strength training, involving resistance against force, is a key component in preventing bone loss, maintaining strength, and reducing the risk of falls (particularly in older adults). Personalised approaches, whether using body weight, resistance bands, or weights, are crucial. It’s useful to aim for 2-3 bouts of strength training each week, and to progressively build this up over time. Post-exercise protein intake within 30 minutes aids muscle repair and overall bone health.
Medications and Hormone Replacement Therapy (HRT)
For some, medications, including Hormone Replacement Therapy (HRT) and specific osteoporosis drugs like bisphosphonates offer valuable options to enhance bone health. HRT at standard doses or above for 2 years duration or more has been shown to prevent osteoporosis related fractures and treat bone loss. Some studies have suggested this benefit may persist for several years after HRT is stopped.
Conclusion
Prioritising bone health is a proactive step toward a healthier and more resilient future. By adopting a holistic approach that includes nutrition, exercise, and lifestyle choices, we can optimise our bone health, supporting active independent living into later life. Noting our bone mass peaks in our 30s, encouraging our young people to keep active can support their bone health too.
