Perimenopause can be a confusing and often overwhelming time for many people, as the symptoms can vary so much, fluctuate over time and mimic many other conditions.
Here’s what you need to know about how to recognise perimenopause, aswell as insights into consulting with your healthcare professional about perimenopause.
Every Person’s Experience is Unique
It’s important to remember that no two experiences of perimenopause are the same. Some people don’t notice much in the way of symptoms at all, while others may experience severe physical and emotional changes. Some might feel relieved when their periods stop, while others may mourn this ending of their menstrual cycles. It can be an isolating time, as friends may go through it at a different time and in a different way.
Common Symptoms of Perimenopause
Here are some of the most common signs to be aware of:
- Changes in Your Cycle: You might notice your periods becoming heavier or lighter, longer or shorter, more frequent or erratic.
- Worsening PMS
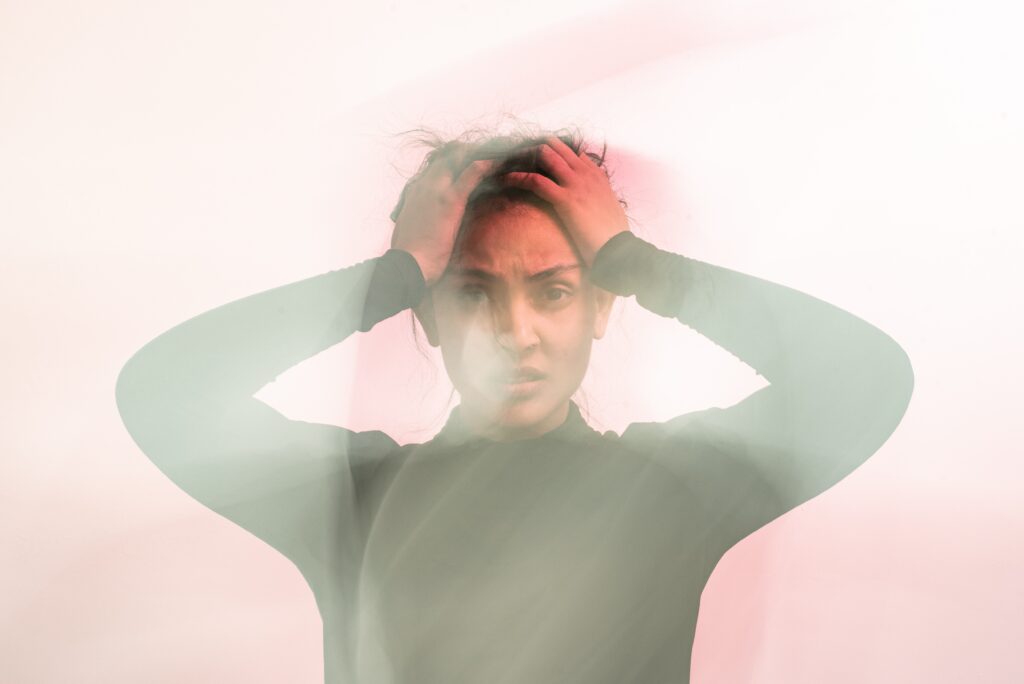
- Mental Health Effects: Anxiety, depression, low self-esteem, and irritability are unfortunately all very common.
- Cognitive Effects: Brain fog and altered concentration can be especially challenging at work.
- Fatigue and low energy
- Sleep Disturbances
- Hot Flushes and Night Sweats
- Vaginal Dryness and Changes in Bladder Function
Less Commonly Known Symptoms
While some symptoms are widely recognized, others can be more subtle and can catch us out:
- Dizziness and Palpitations
- Joint Pain
- Central Weight Gain
- Headaches
- Bloating
- Hair, Skin, and Nail Changes
Symptoms Can Fluctuate
It’s common for perimenopausal symptoms to fluctuate over time. One day you might feel fine, while the next day a symptom may flare up. If you’re experiencing anxiety or low mood, let your healthcare professional know if the symptoms seem intermittent. This fluctuation in mood is often a hallmark of perimenopause. Although the low mood associated with perimenopause can be just as severe as clinical depression, it can also come and go, offering valuable clues to the underlying cause of your symptoms.
Track Your Menstrual Cycle

Keeping track of changes in your menstrual cycle, if you have one, can provide valuable insights into your experience. Even subtle changes, like a cycle shortening from 28 days to 27 days or a period lasting one day longer than usual, can be telling. Tracking these changes over several months can help both you and your healthcare professional understand where you are in the process. If you can, look back at your cycle from a year ago to see if there are noticeable patterns.
You can go old school and use a diary, or ticksheet, or one of the numerous apps now available. I would say though, that some of us can become more anxious by focusing on all that is not going so well. We have enough of a negativity bias as is, so tracking is not for everyone.
Be Open About Your Symptoms
If you suspect that your symptoms are related to perimenopause, it’s okay to let your healthcare professional know. While many signs point to hormonal changes, other underlying conditions might also need to be considered. For example, if you’re experiencing widespread joint pain, your healthcare professional may need to assess whether arthritis is a possibility in addition to menopause. However, if you’ve linked your joint pain to other symptoms like changes in your menstrual cycle or vaginal dryness, this could be a strong indicator that perimenopause is at play.

Online Consultations
In today’s digital age, online consults can be a great tool for sharing your symptoms with your healthcare professional. With the ability to explain your experiences in your own time, they allow you to provide a comprehensive picture of your symptoms. They also give you the opportunity to mention minor symptoms that might otherwise go unreported but that could contribute to the overall diagnosis. Symptoms such as vaginal dryness, low libido, urinary incontinence, or intrusive thoughts can sometimes be difficult to discuss in person, writing them down might make it easier for you to share.
The Role of Healthcare Professionals
Many symptoms of perimenopause can have numerous causes. A person experiencing symptoms like dizziness and palpitations may not immediately connect them to perimenopause, and healthcare professionals must rule out serious conditions, such as heart arrhythmias, whilst also considering menopause as a potential cause.
There is sometimes not enough understanding of the role hormones play, and this is partly due to the biases women face in healthcare. The male body is the default normal body, and the male experience of illness is the one that we learn about at medical school. I started at medical school in 1994. It was only the year before I started, 1993, that it was mandated that women had to be included as participants in research; before that, they were usually excluded as the variability of women’s results complicated everything. So my learning, and a whole generation of clinicians like me, was based on the male experience. This has had significant impacts on women’s health outcomes and research into women’s health. We understand now that women respond differently to drugs and present differently with illnesses, and hormones play a really big role in everything!
And although at medical school I did learn about menopause, I didn’t learn about perimenopause. I learned about menopause affecting women in their 50s whose periods had stopped, not understanding it could affect us much earlier. So, clinicians are on the back foot a bit when it comes to understanding perimenopause. But the situation is improving..
Know Your Options
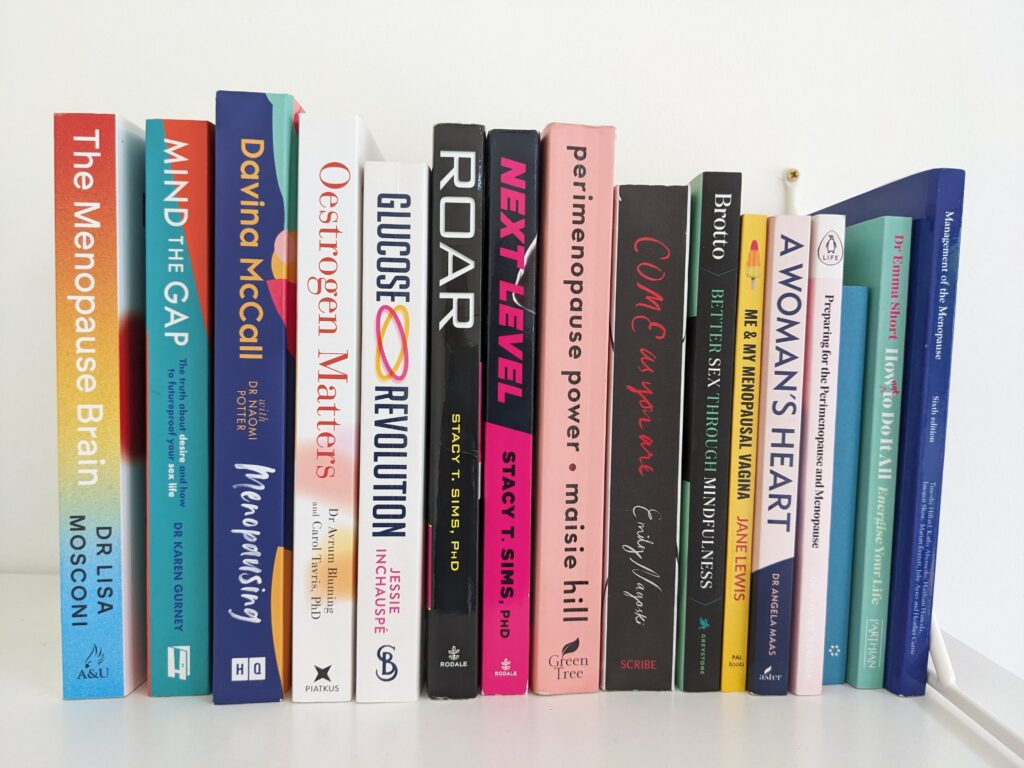
When discussing perimenopause with your healthcare professional, it’s helpful to know what you’re looking for. Are you seeking to understand your symptoms better? Are you interested in exploring lifestyle changes, trying hormone replacement therapy (HRT), or considering non-hormonal treatments? There’s a wealth of information available through books, podcasts, and websites, though it can feel overwhelming. I’ve shared some of my favourite resources on my website, and I’d love to hear about yours, too!
Conclusion
Navigating perimenopause can be challenging, but by staying informed, tracking your symptoms, and working closely with your healthcare professional, you can find the support and solutions that work best for you. Whether you’re exploring lifestyle changes, treatments, or simply seeking understanding, you’re not alone in this journey.
Here at Rethink, my approach is simple – to support you with what you need to thrive at menopause.
Contact me today to find out more.